

Seesaw Nystagmus
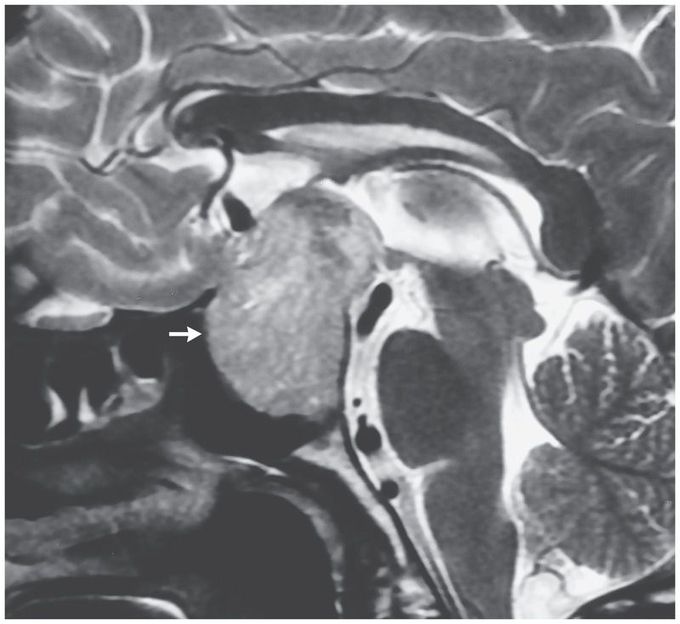
A 52-year-old man presented to the emergency department with a 1-year history of generalized headache, diminished vision, and abnormal eye movements. Examination of the fundus revealed disk pallor. His pupillary reflexes were normal, but there was reduced visual acuity (20/120) in both eyes and bitemporal hemianopia. Ocular examination revealed rhythmic, torsional, and vertical movement in which the eye rotating inward moved up as the other eye moved down, a finding known as seesaw nystagmus. The movement increased in amplitude during downward gaze. Magnetic resonance imaging of the brain revealed a giant pituitary adenoma measuring 48 mm in diameter (arrow), with suprasellar extension that was compressing the optic chiasm. Seesaw nystagmus is a type of pendular nystagmus that has been reported in patients with giant suprasellar lesions that compress the mesodiencephalic region. This form of nystagmus has been attributed to maladaptation of the vestibulo-ocular reflex and a dysfunctional ocular counter-rolling response. This patient had a nonfunctional pituitary macroadenoma with coexisting hypothyroidism and hypogonadism. He underwent a transsphenoidal hypophysectomy, after which there was complete resolution of the nystagmus. On follow-up at 3 months, the visual acuity in both eyes had improved to 20/40.

