

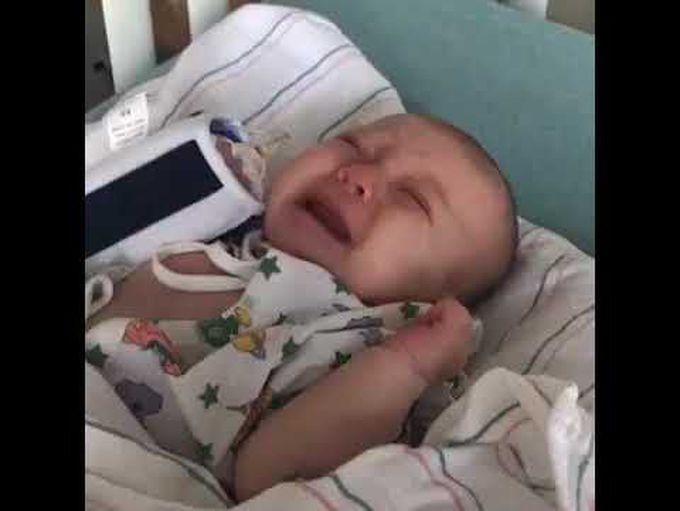
Whooping Cough in a Young Infant
An 8-week-old girl was brought to the hospital with a 2-week history of worsening cough without fever. Her parents heard whooping associated with the coughing and witnessed pauses in her breathing. She had been exposed to a grandmother who had recently had a cough that was thought to be bronchitis. The grandmother’s vaccination history was unknown. The infant’s mother had received tetanus–diphtheria–acellular pertussis (Tdap) vaccination during pregnancy; the infant had not yet been vaccinated, given her age. Physical examination revealed a characteristic whoop associated with the cough (see video). Laboratory results showed a white-cell count of 14,500 per cubic millimeter (reference range, 6900 to 12,800) with lymphocytosis. Polymerase chain reaction performed with a sample of nasopharyngeal aspirate confirmed Bordetella pertussis infection. In young infants, complications of pertussis include apnea, bradycardia, pneumonia, seizures, and death. The patient and her parents and grandmother were treated with azithromycin. During the hospitalization, the patient had recurrent episodes of coughing, apnea, oxygen desaturation to below 50%, and bradycardia (heart rate, 50 beats per minute), which led to the use of bag-mask ventilation as a rescue measure. She also received supplemental oxygen and nasogastric feeding. In total, she was hospitalized for 25 days. On follow-up 3 months after discharge, the patient was well and developing normally, and she did not have a cough.

