

Portal Venous Gas
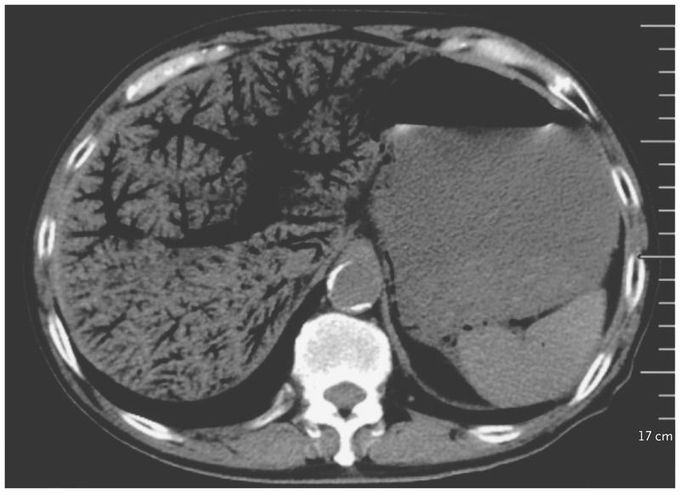
A 72-year-old man presented to the emergency department with an 11-hour history of periumbilical abdominal pain and inability to pass flatus. His medical history included chronic lymphocytic leukemia (for which he had been taking ibrutinib), type 2 diabetes, and chronic hepatitis B virus infection. The pulse was 155 beats per minute, and the blood pressure 83/52 mm Hg. On physical examination, his abdomen was diffusely tender, with the most severe pain in the right upper quadrant. Initial laboratory studies of the blood revealed a white-cell count of 22,570 per cubic millimeter (reference range, 4000 to 10,000), an arterial blood pH of 7.27 (reference range, 7.35 to 7.45), and a lactate level of 8 mmol per liter (72 mg per deciliter) (reference range, 0.5 to 1.7 mmol per liter [4.5 to 15.3 mg per deciliter]). Computed tomography of the abdomen revealed extensive portal venous gas, as well as gas in the bowel wall, which had an appearance consistent with ischemic bowel. Portal venous gas is most commonly associated with bowel ischemia and is a poor prognostic sign in patients with that condition; however, it can also develop in patients with other conditions, such as infection or inflammatory bowel disease, or as a result of an interventional procedure. Treatment was initiated with fluid resuscitation, broad-spectrum intravenous antibiotics, and vasopressors, and an urgent laparotomy was planned. However, the patient’s clinical condition deteriorated rapidly, and he died 2 hours after presentation.
I was diagnosed as a Hepatitis B carrier in 2015, with early signs of liver fibrosis. At first, antiviral medications helped control the virus but over time, resistance developed, and the effectiveness faded. I began to lose hope. In 2021, I discovered NaturePath Herbal Clinic despite my skepticism, I decided to give their herbal treatment a try.To my surprise, after just six months, my blood tests came back negative for the virus.It was nothing short of life-changing.I never expected such incredible results from a natural treatment. But it not only cleared the virus it restored my hope, my health, and my peace of mind.If you or someone you know is battling Hepatitis B, I truly encourage you to explore the natural healing path offered by NaturePath Herbal Clinic. It gave me a second chance and it might do the same for you.www.naturepathherbalclinic.com info@naturepathherbalclinic.com


