

Superior Mesenteric Artery Syndrome
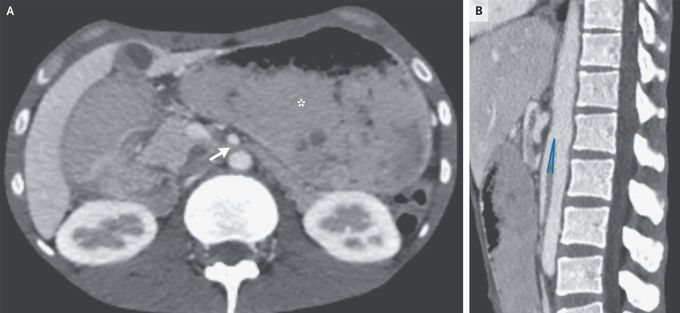
A 26-year-old man from Somalia presented to the emergency department with a 5-month history of dry cough, night sweats, and unintentional weight loss of 18 kg. During this period, epigastric pain and episodes of postprandial vomiting had also developed. His body-mass index (the weight in kilograms divided by the square of the height in meters) was 11. Physical examination was notable for cachexia and abdominal distention with diffuse, mild tenderness to palpation. On the basis of chest imaging and sputum studies, a diagnosis of pulmonary tuberculosis was made. Intravenous antituberculous treatment was initiated, but the patient continued to have postprandial vomiting. Subsequent contrast-enhanced computed tomography of the abdomen showed a paucity of mesenteric and subcutaneous fat, dilatation of the stomach (Panel A, asterisk), and compression of the duodenum between the superior mesenteric artery and the aorta, with an aortomesenteric distance of 3 mm (reference range, 10 to 20) (Panel A, arrow) and an aortomesenteric angle of 7 degrees (reference range, 45 to 60) (Panel B). A diagnosis of superior mesenteric artery syndrome due to cachexia from tuberculosis was made. A nasogastric tube was inserted and parenteral nutrition was initiated; however, the patient opted to leave the hospital after 2 weeks and was lost to follow-up.

