

Idiopathic Pulmonary Hemosiderosis
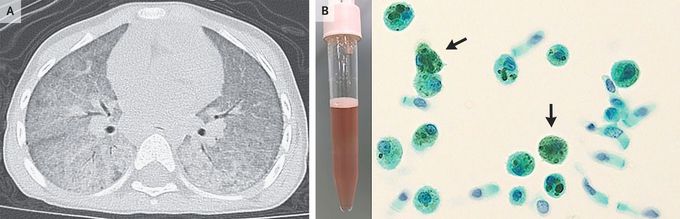
A 3-year-old girl was referred to the pediatric rheumatic disease clinic for recurrent fevers. Three months earlier, she had been hospitalized for fevers and hypoxemia. Her hemoglobin level had been 5.3 mg per deciliter (reference range, 11.6 to 14.8), and computed tomography of the chest had revealed diffuse ground-glass opacities and consolidations (Panel A). No definitive diagnosis had been made. She had received blood transfusions, empirical treatment with antimicrobial agents, and a glucocorticoid. During the tapering of the glucocorticoid dose, the fevers had recurred. At the current presentation, the patient reported no history of hemoptysis. A physical examination was normal. A bronchoscopy with bronchoalveolar lavage was performed. The bronchoalveolar-lavage fluid was reddish-pink, and cytologic examination of the fluid revealed hemosiderin-laden macrophages (Panel B, arrows; Papanicolaou staining). A broad evaluation for causes of diffuse alveolar hemorrhage, including infections, rheumatologic conditions, and congenital heart disease, was negative. A diagnosis of idiopathic pulmonary hemosiderosis — a rare cause of diffuse alveolar hemorrhage — was made. Although this condition classically manifests as hemoptysis, anemia, and abnormal findings on chest imaging, hemoptysis may not be present in children. Systemic symptoms are also present in some cases. The patient received treatment with glucocorticoids and hydroxychloroquine. At a 10-month follow-up visit, her symptoms had abated.

