

Primary Diffuse Meningeal Melanomatosis
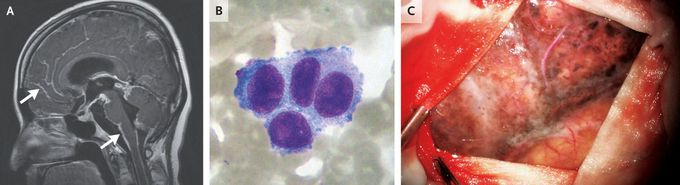
A 27-year-old woman was referred to the neuro-oncology clinic with a 3-month history of headaches, vomiting, confusion, and seizures. The physical examination was notable for meningismus without focal neurologic deficits. Magnetic resonance imaging of the head and whole spine showed diffuse leptomeningeal enhancement on T1-weighted images after administration of contrast material (Panel A, arrows). A lumbar puncture was subsequently performed, and the opening pressure was 330 mm of water (reference range, 80 to 180). Analysis of the cerebrospinal fluid showed a pleocytosis that included abundant large nonhematopoietic cells with a high nuclear-to-cytoplasmic ratio and coarse chromatin (Panel B, Wright–Giemsa stain). Tests for infection were negative. Owing to persistent symptomatic intracranial hypertension, the patient was taken urgently for placement of an external ventricular drain. During the procedure, blackened meninges were seen after the dura mater was opened (Panel C). A biopsy sample of the meninges was consistent with melanoma. No other sites of melanoma were identified on a detailed skin examination, ophthalmologic examination, or whole-body positron-emission tomography–computed tomography. A diagnosis of primary diffuse meningeal melanomatosis — a rare form of primary central nervous system melanoma — was made. Testing for BRAF V600 mutations was negative. Treatment with immunotherapy was initiated, but the patient died 7 months after the diagnosis was made.

