

Encapsulating Peritoneal Sclerosis
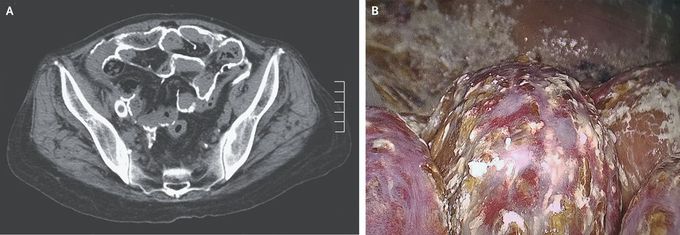
A 52-year-old woman with end-stage kidney disease that was being managed with peritoneal dialysis presented to the nephrology clinic with a 1-month history of bloody dialysate. During her 12 years of undergoing peritoneal dialysis, she had had three episodes of bacterial peritonitis. At the current presentation, she reported no fever or gastrointestinal symptoms. The physical examination was unremarkable. Laboratory studies, including assessments of serum calcium and intact parathyroid hormone levels, were also unremarkable. Computed tomography of the abdomen showed extensive calcification along the visceral and parietal peritoneum (Panel A). Owing to concern for encapsulating peritoneal sclerosis, exploratory laparoscopy was performed to confirm the diagnosis. A markedly thickened parietal peritoneum covered in chalklike deposits was seen (Panel B). Adhesions between the peritoneum and inflamed intestinal serosa were also noted. Histopathological examination showed fibrosis and calcification of the parietal peritoneum, and a final diagnosis of encapsulating peritoneal sclerosis with extensive calcifications was made. Encapsulating peritoneal sclerosis, a rare complication of peritoneal dialysis, involves progressive peritoneal fibrosis. In late stages, the bowel loops may become encased, leading to obstruction. The patient’s peritoneal catheter was removed, and maintenance hemodialysis was initiated. Six months later, she had a partial small-bowel obstruction that resolved with conservative management.

