

Tuberculous Optochiasmatic Arachnoiditis
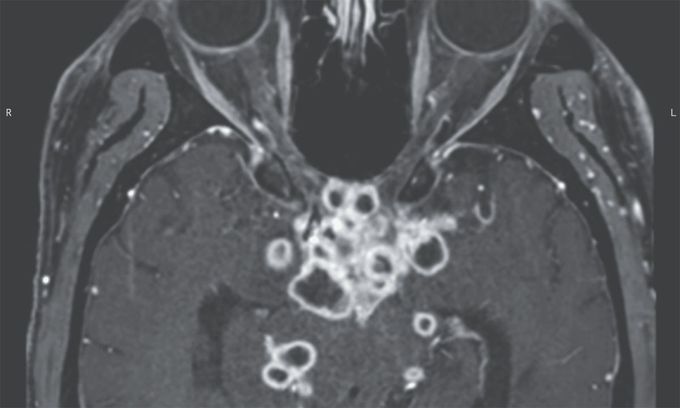
A 29-year-old man presented to the emergency department with a 1-week history of headache and blurry vision. Six weeks earlier, he had received a diagnosis of gastrointestinal tuberculosis and had begun antituberculosis therapy. Physical examination was notable for nuchal rigidity, papilledema, and a relative afferent pupillary defect on the right side. Ophthalmologic evaluation revealed visual acuity of 20/200 in the left eye and only light perception in the right eye. Magnetic resonance imaging of the head revealed multiple ringlike enhancing lesions near the optic chiasm, optic tracts, and perimesencephalic and suprasellar cisterns (see image). Cerebrospinal fluid analysis showed lymphocytic pleocytosis, and nucleic acid amplification testing identified Mycobacterium tuberculosis. A diagnosis of tuberculous optochiasmatic arachnoiditis was made. Tuberculous optochiasmatic arachnoiditis is a complication of tuberculous meningitis in which exudates cause inflammation of the arachnoid of the optic nerve and chiasm, which can result in vision loss. In this patient, the development of this condition was thought to be a paradoxical reaction to antituberculosis therapy that resulted in the development of new lesions. Treatment with dexamethasone was initiated, and the antituberculosis therapy was continued. At a 3-month follow-up visit, the patient’s symptoms had abated.

