

Skin Necrosis after Transarterial Chemoembolization
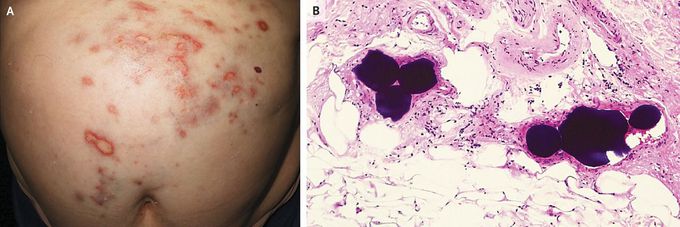
An 81-year-old woman with a history of hepatitis C virus–related cirrhosis and hepatocellular carcinoma was referred to the dermatology clinic owing to a 5-day history of painful, progressively worsening skin lesions over her abdomen. Nine days before presentation, she had undergone transarterial chemoembolization (TACE) with the use of doxorubicin-eluting beads to treat the hepatocellular carcinoma. On examination, there were several erythematous plaques with an atrophic whitish center on the skin of the epigastric region and left upper quadrant (Panel A). Skin biopsy revealed epidermal necrosis and reactive atypia of keratinocytes and eccrine glands, as well as occlusion of small vessels in the reticular dermis by round emboli made up of dense, basophilic material (Panel B; hematoxylin and eosin staining). A diagnosis of skin necrosis due to the drug-eluting beads of TACE was made. In TACE, the spread of chemoembolization material beyond the hepatic-artery vascular territory — also known as nontarget embolization — is a potential complication. Epigastric skin necrosis may occur when there is embolization of the hepatic falciform artery. The patient was treated with oral pentoxifylline and topical glucocorticoids. Six months later, the skin lesions had abated, but residual scarring remained.
I was diagnosed as a Hepatitis B carrier in 2015, with early signs of liver fibrosis. At first, antiviral medications helped control the virus but over time, resistance developed, and the effectiveness faded. I began to lose hope. In 2021, I discovered NaturePath Herbal Clinic despite my skepticism, I decided to give their herbal treatment a try.To my surprise, after just six months, my blood tests came back negative for the virus.It was nothing short of life-changing.I never expected such incredible results from a natural treatment. But it not only cleared the virus it restored my hope, my health, and my peace of mind.If you or someone you know is battling Hepatitis B, I truly encourage you to explore the natural healing path offered by NaturePath Herbal Clinic. It gave me a second chance and it might do the same for you.www.naturepathherbalclinic.com info@naturepathherbalclinic.com


