

Cholesterol Pericarditis
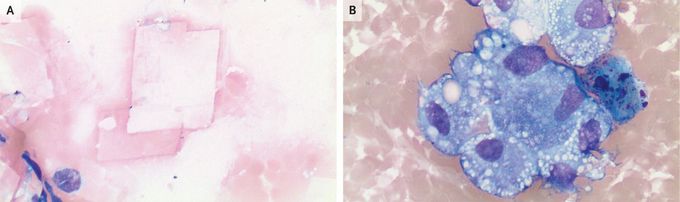
A 64-year-old man with well-controlled rheumatoid arthritis presented to the emergency department with a several-month history of fatigue and a 1-day history of abdominal pain that worsened with deep breathing. At presentation, the heart rate was 105 beats per minute and the blood pressure was 138/95 mm Hg. The physical examination revealed mild abdominal tenderness in the right upper and lower quadrants. Computed tomography of the abdomen showed no major intraabdominal findings but did reveal a large pericardial effusion, which was confirmed on a subsequent transthoracic echocardiogram. Pericardiocentesis was performed, and 960 ml of yellow, cloudy fluid was removed. Studies of samples of the pericardial fluid revealed a lactate dehydrogenase level of 1056 IU per liter (reference range, 100 to 250) and a white-cell count of 2992 per cubic millimeter (reference value, <500). Microscopy of the fluid sample showed cholesterol crystals (Panel A) and foamy histiocytes (Panel B). A diagnosis of cholesterol pericarditis was made. Cholesterol pericarditis is characterized by a chronic pericardial effusion with high levels of cholesterol, which may crystallize in the fluid, and has been associated with rheumatoid arthritis. Treatment with colchicine was initiated, and the effusion did not recur during the patient’s hospital stay. A repeat echocardiogram 3 months after discharge showed no reaccumulation of fluid.

