

Sclerokeratitis in Granulomatosis with Polyangiitis
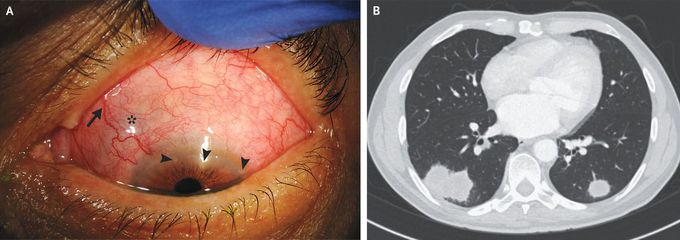
A 68-year-old man presented to the ophthalmology clinic with a 2-month history of pain, redness, blurry vision, and sensitivity to light in both eyes. Over the preceding year, he had also had a dry cough, sinusitis, and unintentional weight loss of 6.8 kg. Eye examination revealed dilated and inflamed scleral vessels (Panel A, arrow); scleral thinning with visible, bluish uveal tissue (asterisk); and peripheral corneal infiltrates (arrowheads). A titer of antineutrophil cytoplasmic antibodies with a cytoplasmic staining pattern (c-ANCA) was 1:640 (reference value, <1:20), and an enzyme-linked immunosorbent assay for the anti–proteinase 3 level showed 1227 U per milliliter (reference range, 0 to 19). Serum creatinine testing and urinalysis were normal. A computed tomographic scan of the chest showed pulmonary nodules (Panel B). Referrals to the rheumatology and pulmonology departments were made. A lung-biopsy specimen showed necrosis with vasculitis and foci of acute inflammation with multinucleated giant cells, findings that confirmed a diagnosis of granulomatosis with polyangiitis. Ocular manifestations of granulomatosis with polyangiitis include scleritis, keratitis, optic neuropathy, and retinal vasculitis. Prompt diagnosis and treatment are critical to prevent vision loss and other systemic complications. Treatment with topical and systemic glucocorticoids and rituximab was initiated, and the patient’s symptoms abated.

