

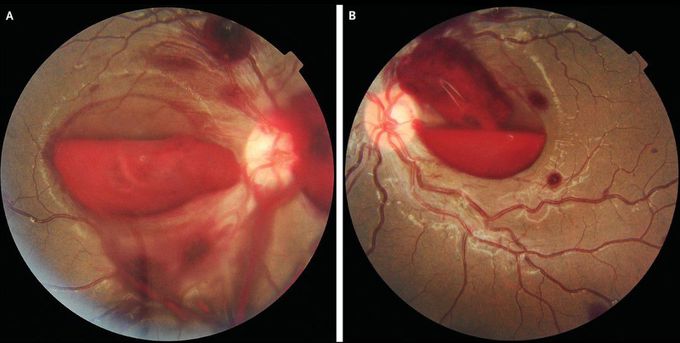
Retinal Hemorrhages in Leukemia
A 14-year-old boy with acute lymphoblastic leukemia presented to the emergency department with a 2-week history of fatigue and fever and 3 days of blurry vision. He had been receiving maintenance chemotherapy for his leukemia. Before the onset of his current symptoms, the patient had had no history of vision problems, and he had no recent history of eye trauma, severe coughing, or vomiting. Examination of both eyes revealed a visual acuity limited to counting fingers, retinal venous congestion, large preretinal hemorrhages in the maculae, and scattered peripheral intraretinal hemorrhages (Panel A, right eye; and Panel B, left eye). A complete blood count showed a white-cell count of 1600 per cubic millimeter (reference range, 4000 to 10,000), a hemoglobin level of 6.9 g per deciliter (reference range, 12 to 16), and a platelet count of 15,000 per cubic millimeter (reference range, 150,000 to 400,000). Retinal hemorrhages may occur as a manifestation of leukemia or a complication of therapy; the former may be triggered by hyperviscosity, coagulopathy, leukemic infiltration, or vessel damage, whereas the latter is triggered by severe anemia and thrombocytopenia. The patient was treated with broad-spectrum antimicrobial agents and transfusions of platelets and packed red cells. At follow-up 4 months later, his visual acuity had improved to 20/30 in both eyes.

