

Gastrointestinal Amyloidosis
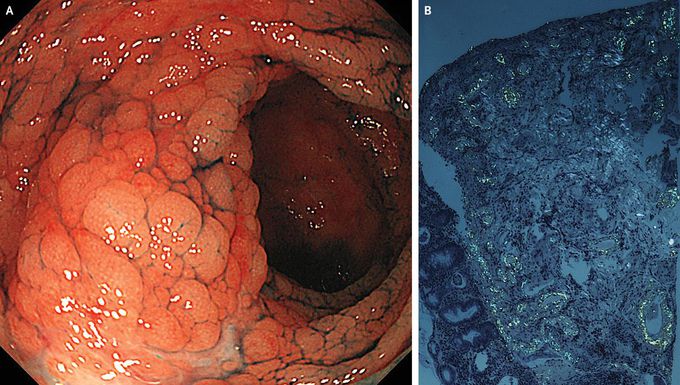
A 60-year-old woman presented to the rheumatology clinic with a 3-month history of diarrhea, nausea, and anorexia. She had a 35-year history of rheumatoid arthritis, for which she was receiving methotrexate and tacrolimus; however, disease activity was not well controlled. Physical examination showed swelling and tenderness in the metacarpophalangeal joints and the wrists. Upper and lower gastrointestinal endoscopy revealed edematous, granular lesions with erosions in the ascending and transverse colon (Panel A). Biopsy specimens showed amyloid deposits with apple-green birefringence on Congo red staining under polarized light (Panel B). A diagnosis of gastrointestinal AA amyloidosis associated with a high activity level of rheumatoid arthritis was made. AA amyloidosis, which is caused by the extracellular deposition of amyloid fibrils derived from serum amyloid A protein, is also associated with a number of other chronic inflammatory conditions, including juvenile idiopathic arthritis, ankylosing spondylitis, Crohn’s disease, and familial Mediterranean fever. Treatment with tocilizumab, a monoclonal antibody against interleukin-6 receptor, was initiated. Within several days after the initiation of therapy, the patient had a reduction both in the gastrointestinal symptoms and in joint pain and swelling.

