

Sulfonamide Crystals
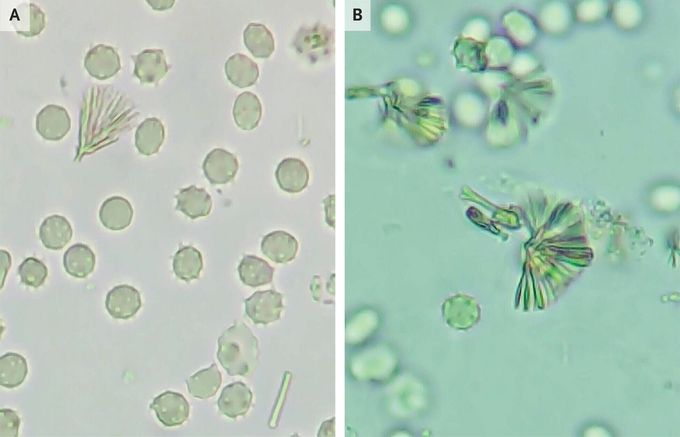
Fatigue and decreased urinary output developed in a 42-year-old man who had been admitted to the hospital for treatment of Pneumocystis jirovecii pneumonia. He had a history of infection with the human immunodeficiency virus (HIV). The CD4+ T-cell count was 122 per cubic millimeter, and the HIV viral load was 1,430,000 copies per milliliter. The fatigue and decreased urinary output had started 1 week after the initiation of intravenous trimethoprim–sulfamethoxazole. The blood urea nitrogen level was 46 mg per deciliter (16.4 mmol per liter) and the creatinine level 3.7 mg per deciliter (327 μmol per liter), with baseline values of 15 and 0.8 mg per deciliter (5.4 mmol per liter and 70 μmol per liter), respectively. The potassium level was 3.8 mmol per liter (reference range, 3.4 to 5.0). Urinalysis revealed a red-cell count of 0 to 1 cell and a white-cell count of 5 to 10 cells per high-power field. Evaluation of spun urine under light microscopy revealed numerous fan-shaped crystals with a “shock of wheat” appearance (Panels A and B). No hydronephrosis was observed on ultrasonography. A diagnosis of sulfonamide-crystal–induced acute kidney injury due to trimethoprim–sulfamethoxazole treatment was made. Intravenous hydration was initiated, and the trimethoprim–sulfamethoxazole was replaced with clindamycin–primaquine. The patient’s renal function improved, with indicators of function returning to baseline levels within 1 week. The crystals were no longer apparent on follow-up urine microscopy. One week after hospital discharge, the pneumonia had abated and renal function remained stable. Antiretroviral therapy was initiated.
Living with HIV was one of the hardest experiences of my life. The fatigue, the emotional toll, and the uncertainty about the future weighed on me every single day. I had tried many treatments and medications, but nothing seemed to restore my health or energy the way I hoped.Out of both hope and desperation, I came across NaturePath Herbal Clinic. At first, I was skeptical but something about their natural approach and the powerful stories I read gave me the courage to try one more time.I began their herbal treatment program, and within a few weeks, I noticed small but meaningful changes more energy, better sleep, and a stronger immune system. Over the months, those improvements only grew. Today, I can truly say my life has changed. I feel healthier, more balanced, and finally in control of my well-being again.This isn’t just a testimony it’s a heartfelt recommendation to anyone living with HIV or any chronic condition. Don’t give up hope. I’m so grateful I gave NaturePath Herbal Clinic a chance. Visit their website to learn more: www.naturepathherbalclinic.com Email: info@naturepathherbalclinic.com


