

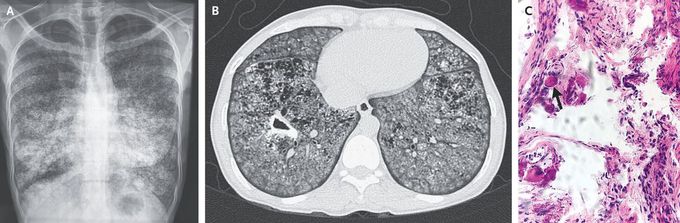
Pulmonary Alveolar Microlithiasis Complicated by Tuberculosis
A 36-year-old woman presented to the outpatient clinic with a 2-month history of fever, night sweats, cough, and worsening shortness of breath. On examination, her oxygen saturation was 88% while she was breathing ambient air. A chest radiograph showed widespread fine micronodular opacities with a “sandstorm” appearance (Panel A). Computed tomography of the chest revealed calcified micronodules, ground-glass opacities, and a cavitation (Panel B). A sputum smear was negative for acid-fast bacilli. Subsequently, a transbronchial biopsy was performed, and pathological examination of the tissue revealed microliths (Panel C, arrow). The bronchial aspirate was positive for Mycobacterium tuberculosis. Testing for human immunodeficiency virus antibodies was negative. A diagnosis of pulmonary alveolar microlithiasis complicated by tuberculosis was made. The patient began treatment for tuberculosis. Four weeks later, the fever, night sweats, and cough had abated, but her shortness of breath persisted. Lung transplantation — the only established treatment for pulmonary alveolar microlithiasis — was not an available intervention in this case owing to resource constraints.

