

Tracheal Agenesis with Bronchoesophageal Fistula
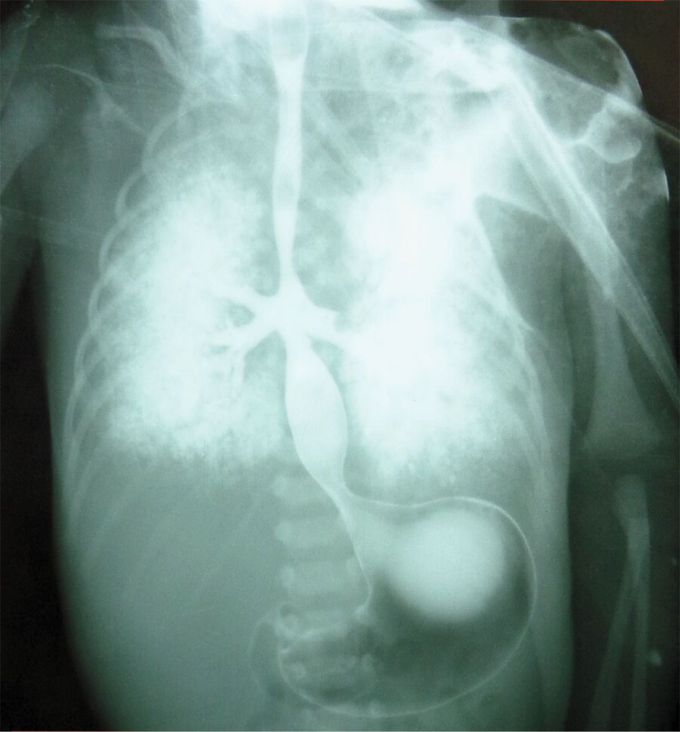
Cyanosis and respiratory distress developed in a neonate after delivery at 32 weeks of gestation. His mother had not received regular antenatal care. Endotracheal intubation and tracheostomy were attempted without success, and bag-valve–mask ventilation was performed, but the boy died from respiratory failure 4 hours after delivery. An esophagram obtained post mortem, after the administration of barium, suggested tracheal agenesis and bronchoesophageal fistula. An autopsy confirmed absence of the trachea, with fusion of the main bronchi and bronchoesophageal fistula, findings consistent with a diagnosis of type II tracheal agenesis, defined in accordance with the Floyd classification system. Additional findings included dysmorphic facial features, a double superior vena cava, an ostium secundum atrial septal defect, and a horseshoe kidney. Postnatal karyotyping revealed trisomy 18. Diagnostic advances, including those enabling assessment of the fetus on sonography and magnetic resonance imaging, have facilitated the establishment of this diagnosis prenatally.

