

Vein of Galen Malformation
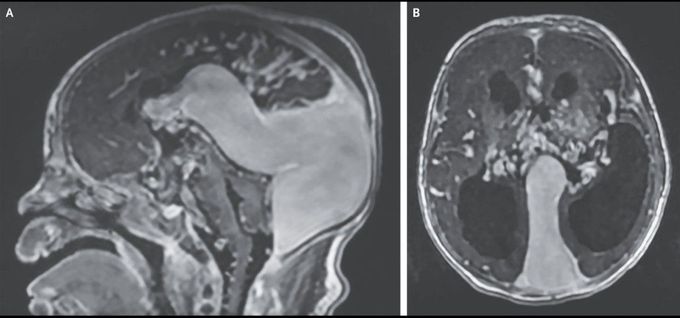
A neonate born at 37 weeks of gestation had respiratory distress 3 hours after birth. A physical examination was notable for subcostal retractions, coarse breath sounds in both lungs, and a systolic murmur. A chest radiograph showed cardiomegaly and bilateral pleural effusions, and an echocardiogram showed a patent foramen ovale, a dilated right atrium, a dilated and hypertrophied right ventricle, tricuspid regurgitation, and right-to-left shunting at the patent ductus arteriosus. Cranial ultrasonography and gadolinium-enhanced T1-weighted magnetic resonance imaging revealed a large choroidal type of vein of Galen malformation, hydrocephalus, and atrophy of the brain stem and cerebellum in the sagittal (Panel A) and axial (Panel B) views. Vein of Galen malformations are rare congenital arteriovenous fistulas in the brain that can result in heart failure and pulmonary hypertension in neonates. Supportive and endovascular treatments have been shown to prolong survival, but the prognosis remains poor with varying neurodevelopmental outcomes. The patient underwent staged endovascular embolization of the malformation. Despite treatment, which also included mechanical ventilation and the use of vasopressors, inhaled nitric oxide, diuretic agents, and prostaglandin E1, the patient had worsening pulmonary edema, liver failure, and renal failure and died 21 days after birth.

