

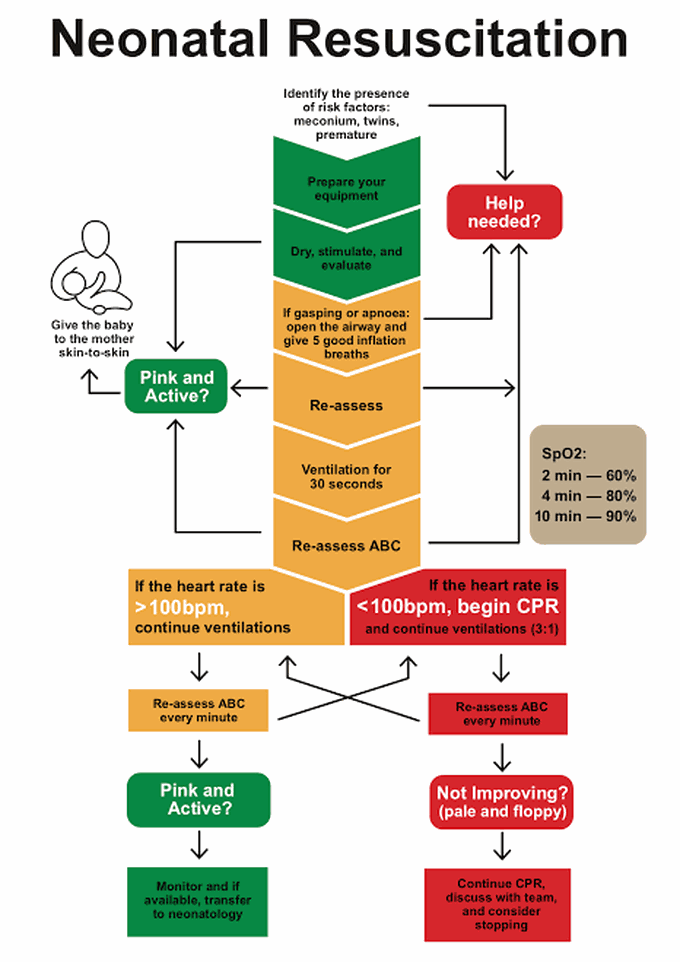
Steps of neonatal resuscitation
1 - Stimulate the neonate by drying Tactile stimulation can trigger spontaneous breathing. It is done by drying the neonate. If the neonate starts to breathe or cry within 5 seconds, proceed to routine care (Section 10.1). If not, stop stimulation and proceed to step 2. 2 - Clear the airway Lay the neonate on the back with the head in a neutral position (Figure 10.1); avoid flexion or hyperextension of the neck, as this can obstruct the airway. 3 - Stimulate the neonate Rub the back and the soles of the feet vigorously but not roughly (do not shake, slap or hang the infant by the feet, etc.). If the neonate is having difficulty breathing or still not breathing after 5 seconds: stop active stimulation, and proceed to steps 4 and 5. 4 - Clamp and cut the cord If not already done, clamp and cut the cord. 5 - Perform bag-mask ventilation (room air) Fit the mask over the nose and mouth. Press firmly to prevent air leaks. Hold it with one hand, with the thumb on one side and the index and middle fingers on the other (Figures 10.2 and 10.3). With the other hand, squeeze the bag at a rate of 30 to 60 breaths/minute for 60 seconds. Ventilation is effective if the chest rises and falls. Attention, excessive ventilation pressure can cause a pneumothorax. If the chest fails to rise: – Check the connection between the bag and the mask; – Correct the position of the mask on the face; – Correct the head position. 6 - Oxygenation If oxygen is available: connect the ambu bag to an oxygen reservoir after 2 minutes of ventilation, setting it at a 2 litres/minute flow rate. Ventilation is a priority and should not be interrupted to connect the oxygen (have an assistant connect the oxygen). Stop resuscitation if the neonate has: – No heart rate after 10 minutes. – No spontaneous respiration after 20 minutes of effective ventilation, even if the heart rate is adequate.

