

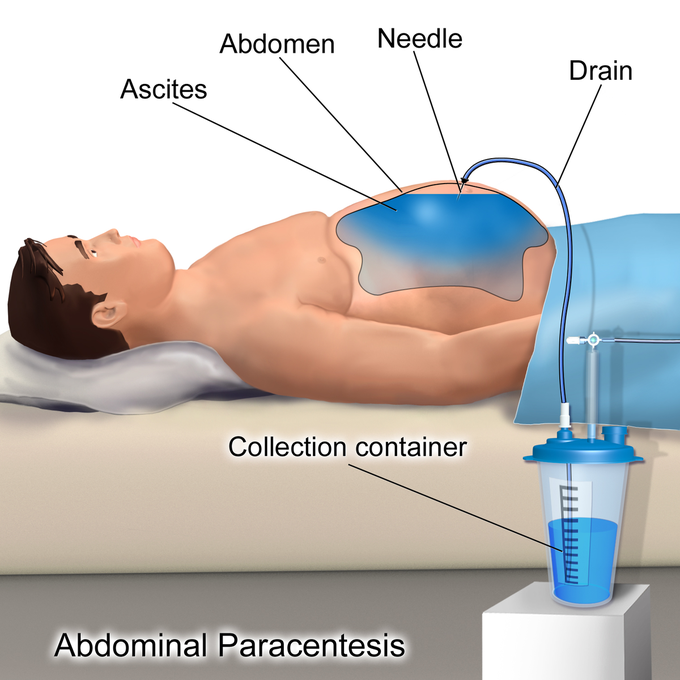
Paracentesis or Ascitic tap
Causes of transudative ascites include the following: ➢ Hepatic cirrhosis ➢Alcoholic hepatitis ➢Heart failure ➢Fulminant hepatic failure ➢Portal vein thrombosis Causes of exudative ascites include the following: ➢Peritoneal carcinomatosis ➢Inflammation of the pancreas or biliary system ➢Nephrotic syndrome ➢Peritonitis ➢Ischemic or obstructed bowel INDICATIONS Diagnostic tap is used for the following: ➢New-onset ascites - Fluid evaluation helps to determine etiology ➢ differentiate transudate versus exudate ➢ detect the presence of cancerous cells, or address other considerations ➢Suspected spontaneous or secondary bacterial peritonitis Therapeutic tap is used for the following: ➢Respiratory compromise secondary to ascites ➢Abdominal pain or pressure secondary to ascites (including abdominal compartment syndrome) EQUIPMENTS ➢ Sterile gloves and gown ➢ Dressing pack containing gauze and sterile drape ➢ Anti-septic skin preparation ➢ 5ml 1% lidocain ➢ 25G(orange) needle ➢ 21G(green) needle * 2 ➢ 10ml disposable syringe ➢ 20ml disposable syringe ➢ Adhesive dressing ➢ Universal containers * 3 ➢ Blood culture bottles PROCEDURE Posting below..... COMPLICATIONS ➢ Significant bleeding ➢ Infection ➢ Renal failure ➢ Hyponatremia ➢ Hepatic encephalopathy ➢ Complicated bowel perforation ➢ Paracentesis leak CONTRAINDICATIONS ➢ An acute abdomen that requires surgery is an absolute contraindication. ➢ Severe thrombocytopenia (platelet count less than 20 × 103/μL) and coagulopathy (international normalized ratio INR > 2.0) are relative contraindications. ➢ Pregnancy ➢ Distended urinary bladder ➢ Abdominal wall cellulitis ➢ Distended bowel ➢ Intra-abdominal adhesions
PROCEDURE Prior to tap Before tapping, there are certain investigations that should be undertaken: ➢FBC and clotting screen - if thrombocytopenia is present and severe, most clinicians would give pooled platelets to reduce the risk of bleeding. Fresh frozen plasma may be used if there is evidence of coagulopathy. ➢U/E, creatinine, and LFTs. ➢Abdominal ultrasound - this is not always necessary prior to tap. It is used to review liver, pancreas, spleen and lymph nodes. Ultrasound is a very sensitive means of assessing the extent of ascites and may also show the causative pathology such as carcinoma of ovary or metastatic liver disease. Technique ➢Check that the correct equipment has been assembled: ➢Explain the procedure to the patient, including risks, and obtain consent. ➢Position the patient, usually in the supine position with the head of the bed elevated to allow fluid to accumulate in the patient's lower abdomen. Position of the tap: ➢Locate area of flank dullness lateral to the rectus abdominis muscle and go approximately 5 cm superior and medial to the anterior superior iliac spines. ➢Avoid the inferior epigastric vessels which run up the side of the rectus abdominis to anastomose with the superior epigastric vessels coming down. ➢Avoid the pelvic area, solid tumour masses, prominent superficial veins (caput medusa) and scars (may have collateral vessels close by or adherent bowel beneath). ➢Using local anaesthetic if needed, the needle is inserted and fluid aspirated. ➢If this does not work then ultrasound guidance may help, especially for a small amount of ascites. ➢10-20 ml of fluid can be aspirated for diagnostic purposes. ➢If a therapeutic tap is required, an IV cannula is placed using the Z track technique. This involves puncturing the skin perpendicularly and advancing the needle obliquely in subcutaneous tissue. This reduces leakage following the procedure, as the puncture site on the skin and the peritoneum are not adjacent. ➢Once the cannula is in place the needle is withdrawn and a giving set and collection bag connected. Drain for 6-8 hours and then remove the cannula or catheter and cover with a simple adhesive bandage. ➢Swift drainage is safest but if the patient develops symptoms of hypotension then the drainage may need to be slowed or prematurely terminated. ➢Large volumes can be taken off within 2-4 hours but this can reduce both the intra-abdominal and inferior vena cava pressure. In response the cardiac output may increase. This may lead to a reduction in blood pressure and should be anticipated at the outset. In practice colloid replacement is usually given.

