

Atrioventricular Dissociation during Ventricular Fibrillation
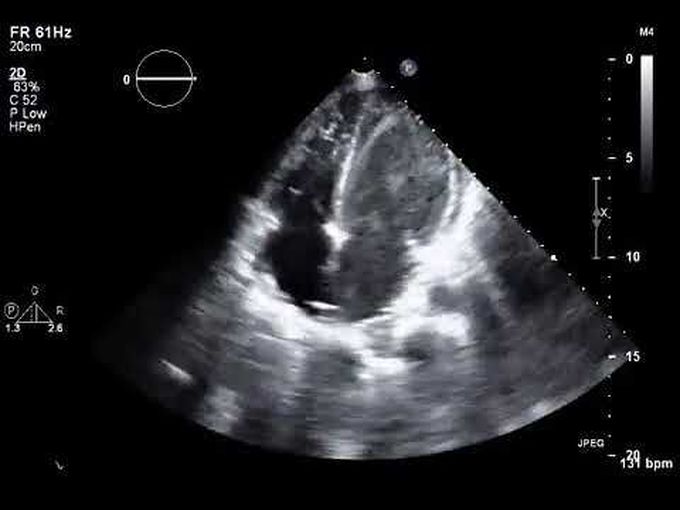
A 50-year-old woman with a history of bicaval cardiac transplantation presented to the emergency department with a 1-week history of dyspnea, fatigue, and weight gain. A transthoracic echocardiogram showed newly reduced left ventricular systolic function, and an endomyocardial biopsy confirmed acute cellular rejection of the transplanted heart. Her hemodynamic status deteriorated, thereby prompting initiation of venoarterial extracorporeal membrane oxygenation. Sustained ventricular fibrillation developed (Panel A, green tracing), with a loss of right and left ventricular contractility, as indicated by a nonpulsatile pulmonary arterial waveform (Panel A, yellow tracing) and systemic arterial waveform (Panel A, red tracing). A regular pulsatile central venous waveform was observed (Panel A, blue tracing and asterisks). Repeat transthoracic echocardiography confirmed near ventricular standstill with a left ventricular thrombus (Panel B, arrow; and video) and preserved right atrial contractility with tricuspid valve opening (corresponding to the central venous waveform). This observation, coupled with concomitant mitral valve opening, indicated atrioventricular dissociation during ventricular fibrillation. Premature closure of the atrioventricular valves immediately after atrial contraction was also observed. The patient had worsening multiorgan failure and died 1 week after presentation.


