

Time is Money: Timely Prophylaxis of VTE in Trauma Patients
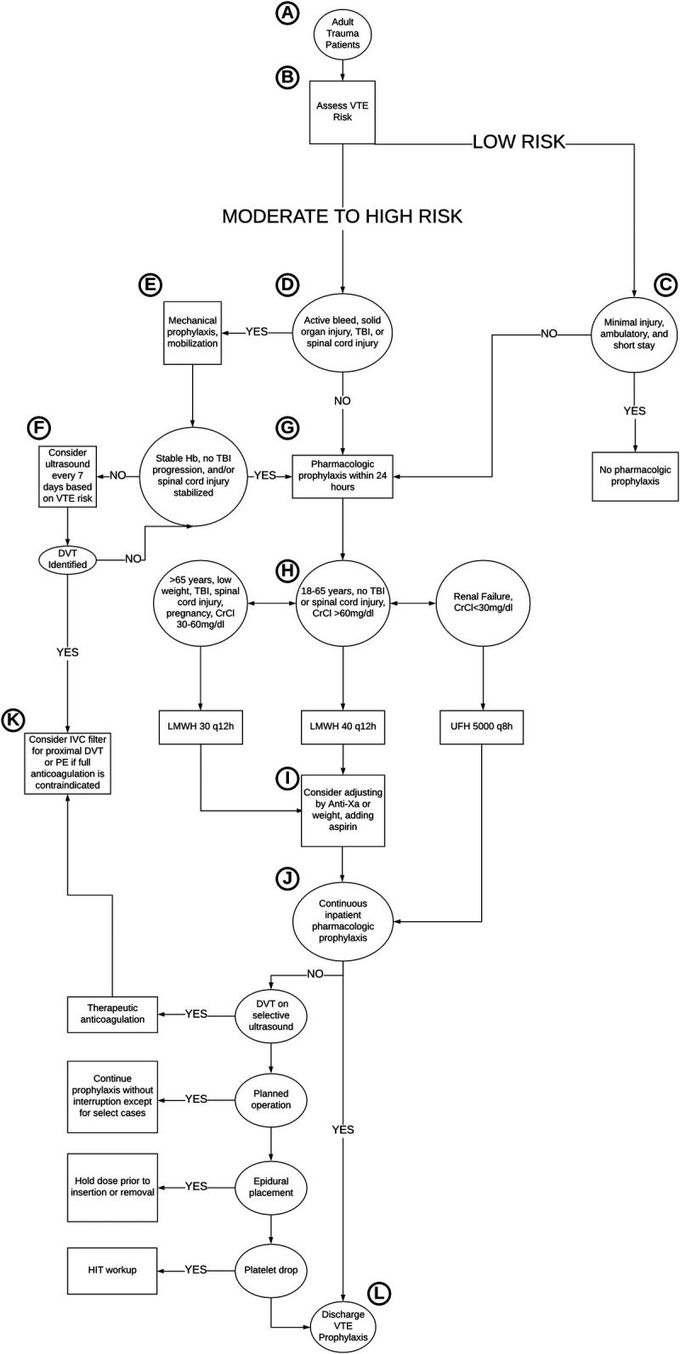
Prevention of venous thromboembolism in trauma patients remains one of the biggest challenges in trauma management. Deep vein thrombosis (DVT) and pulmonary embolism (PE) are potentially preventable conditions, provided timely assessment of risk factors and administration of prophylactic anticoagulants are ensured. Updated guidelines by Western Trauma Association (WTA) devised an algorithm for step wise identification of at-risk patients and subsequent treatment, helping in timely decision making according to extent and severity of trauma. According to the guidelines, an Injury Severity Score (ISS) of more than 10 warrants administration of prophylactic anticoagulants, preferably enoxaparin, as soon as possible. For ISS less than 10, other risk factors for venous thromboembolism like advancing age, lower extremity trauma and obesity should be considered, and subsequent prophylaxis should be initiated. Ambulatory patients and those with minor trauma may not require prophylaxis. Delay in administrating anticoagulants may be indicated in patients with active hemorrhage, coagulopathy, and brain and spinal injuries. When it comes to risk of venous thromboembolism in trauma patients, time is legit money. It is imperative to ensure that VTE prophylaxis should be administered within 24 hours of hospital admission. Delay in decision making and administration of prophylaxis may result in DVT and PE. Reference: Updated guidelines to reduce venous thromboembolism in trauma patients: A Western Trauma Association critical decisions algorithm https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7587238/ Image taken from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7587238/

